Cardiovascular Assays
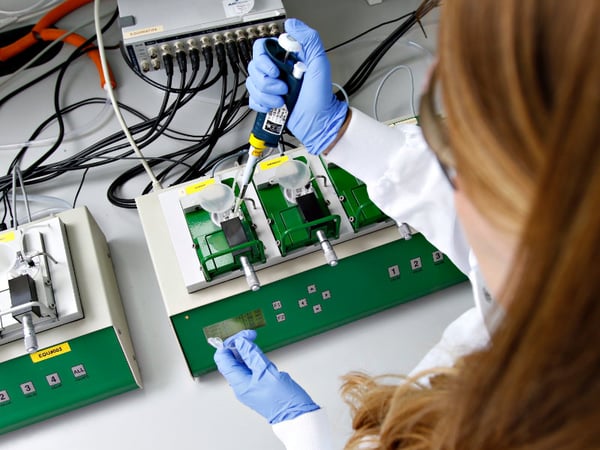
Our selection of human cardiovascular intact fresh tissue models offers a unique insight into the likely effects of your test article in the clinic. Our scientists create customized protocols that answer your specific questions about the effects of test drugs on human cardiac or vascular function using fresh intact blood vessels or cardiac muscle donated via our extensive network of clinical partners from across the UK and USA. The functional tissues are transported rapidly to our pharmacology labs in the USA or UK where our experience scientists are on hand to conduct ex vivo experiments. We can also conduct comparative studies in other preclinical species to explore species differences using the same blood vessels or cardiac tissues.
For regulatory safety pharmacology studies in accordance with ICH S7A, we offer the ability to conduct studies in accordance with Good Laboratory Practice (GLP) and are the only GLP CRO using human fresh, functional, intact tissues.
Explore our Cardiovascular Assays

5-HT
Human tissue testing is an invaluable tool for drug discovery research, allowing you to gather human data before clinical trials, offering insights into drug responses and off-target effects on cardiovascular tissues. Our scientists specialize in testing the effects of compounds on human blood vessels, providing a critical bridge between preclinical and clinical research phases.

Subcutaneous Resistance Arteries
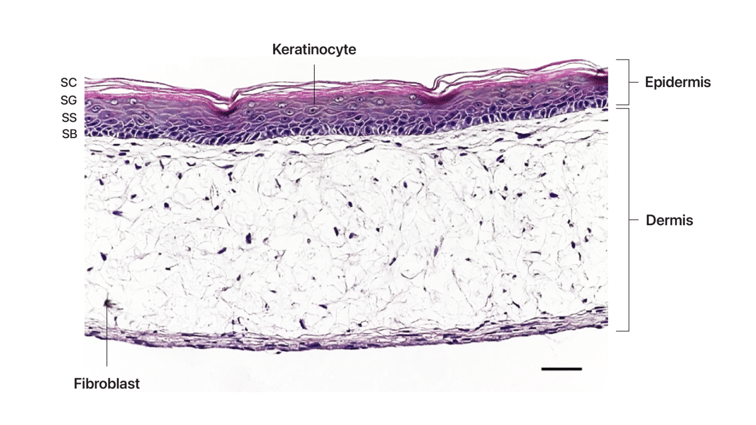
Our state-of-the-art assays focus on subcutaneous resistance arteries, offering critical insights into drug effects on peripheral vascular resistance and systemic blood pressure regulation. Subcutaneous arteries and arterioles, which lie beneath the dermis, play a pivotal role in determining total systemic peripheral vascular resistance (TPR). These small vessels, capable of significant dilation and constriction, are key to understanding vascular control mechanisms.

Cardiac Contractility
Cardiac contractility is of major interest in safety pharmacology, as a number of drugs have been shown to have direct effects on cardiac function that may affect stroke volume and hence cardiac output. Using human isolated fresh cardiac tissues, we can assess your test articles for undesired or off-target effects, or assess their ability to modulate cardiac contractility as potential treatments for heart failure.
Pulmonary Artery Tone
The pulmonary arteries carry deoxygenated blood to the lungs and are essential for healthy respiratory function. Our organ bath model can measure changes in the vascular tone of these arteries in response to your test articles. This diverse test system can estimate a range of function endpoints ex vivo.

Coronary Arteries
The coronary arteries supply blood to the myocardium of the heart and are a key consideration in cardiovascular safety assessment; even small drug-mediated changes in the vascular tone of coronary arteries could increase the risk of angina or myocardial infarction. We are able to assess the potential for drug-mediated effects on human isolated coronary arteries and provide comparisons to coronary arteries from commonly used preclinical species.