Human skin biopsies are small — usually no more than a few millimeters in diameter. Yet they are also highly complex, containing several pathways and cells relevant to skin disease research. An increasing number of scientists are adding ex vivo research to their preclinical portfolio to enhance the translatability of their research. In this article, we will explain how you can join them.
Video: Prefer to watch a video than read? This blog originated as a transcription of our webinar "The REPROCELL Tissue Network: Facilitating Drug Development." Watch the original video above or on REPROCELL YouTube.
How to access human skin biopsies
Skin biopsies can be accessed from three key supply routes: surgery, transplant, or dedicated sampling (clinical biopsies). Dedicated sampling provides small biopsies, while surgical residual tissues arrive as larger pieces of tissue. The route chosen will depend on the assay type, cohort criteria, endpoint criteria, and any ethical considerations. Before beginning, it is vital to ensure that protocols meet the individual study requirements of the clinical site. All types of skin biopsies are suitable for ex vivo culture, meaning they can be kept alive outside of the body to investigate drug efficacy.
Skin tissue residual to surgery or via transplant networks
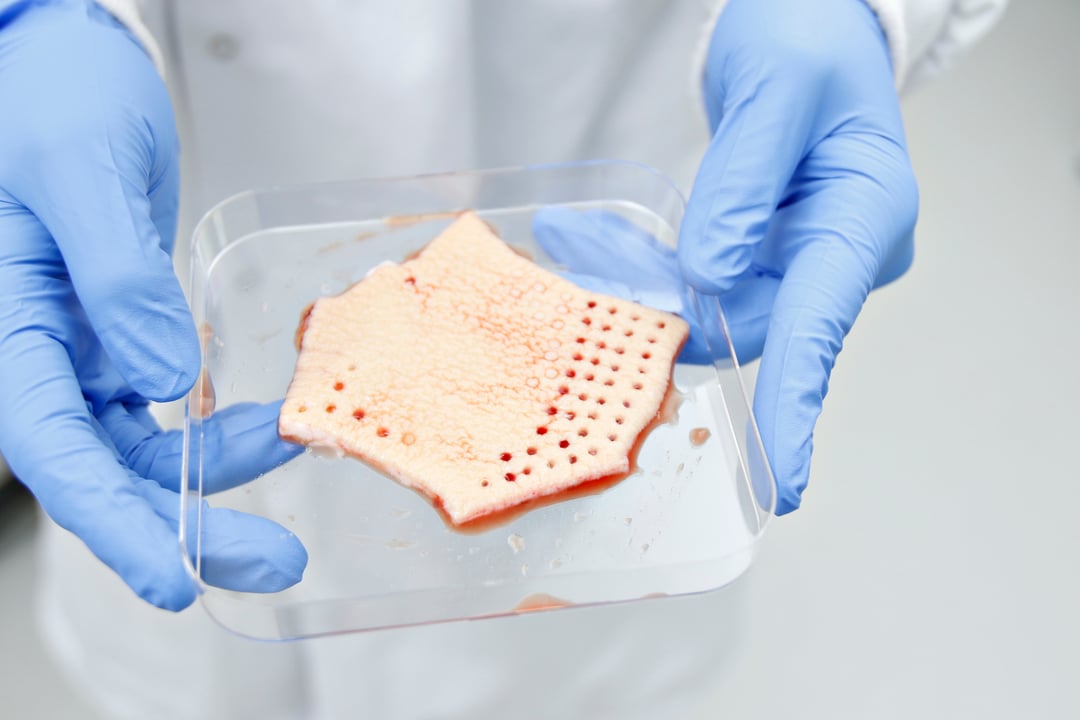
Substantial sections of skin tissue can be obtained via surgery or transplant. Tissue sections are full-thickness, usually from healthy individuals, and can be procured with or without the attached subcutaneous fat layer. This full-thickness tissue can be used to dissect resistance arteries for vascular studies or prepare multiple full-thickness skin biopsies of almost any size. Typically, 3 mm healthy skin biopsies are used in projects investigating systemic drug applications.
These resections are collected in a specialised transport medium and are shipped to the lab within 1-6 hours, depending on the site location. It's important that labs are open and staff are available 24 hours a day, 7 days a week, as tissue samples can arrive at any time.
Akin to a clinical trial, patient selection criteria can be applied to surgical or transplant collections depending on research needs - e.g., sex, age, or ethnicity - and access to deidentified clinical information can provide further valuable insights.
Clinical biopsy sampling for skin disease research
For skin disease research, clinical biopsy (dedicated) sampling may be more appropriate than tissues from surgery or transplant. Donors are recruited via out-patient clinics or clinical trial units on an individual study basis. As with the surgical route, donor criteria and screening can be applied depending on research needs. Ethical restrictions do limit the number and size of any samples collected via this route, but donors can be recruited based on disease type or severity - for example, atopic dermatitis donors (AD or eczema) with a particular EASI score (eczema area and severity index). In general, three biopsies can be taken per patient, which are generally around 3 mm in size. Because this is a dedicated sampling process, it is usually possible to perform additional sampling for blood/urine and to request photographs of lesions if required.
From a biology perspective, patient biopsies achieved via dedicated sampling are the gold standard model of local disease biology. And while the number of biopsies you can obtain from a patient is limited, it is quite easy to scale to a high number of donors. As long as there are not too many stipulations on patient criteria, clinics usually find it easy to recruit patients for sample donation. Using biopsies from dedicated sampling also offers the opportunity to investigate lesional and non-lesional skin from the same donor.
Figure 1: One of the benefits of sourcing residual human skin via surgery or transplant is that a larger number of punch biopsies can be generated from these samples compared to dedicated sampling.
How skin biopsies can be cultured ex vivo in the lab
A large amount of useful data can be generated from ex vivo skin samples, including protein release, gene expression, transcriptomics, proteomics, and immunohistochemistry data. Because these are human systems, genomic profiles of the patient can reveal relationships between genomics and functionality e.g., why do some patients respond to treatment and others do not? Without detailing all of the options, we have highlighted examples of human skin models commonly used in drug development below.
Ex vivo skin disease models
The benefit of using ex vivo skin disease models is that they are highly clinically and disease-relevant. For the study of local skin biology, there's no other preclinical model that compares to testing in living human skin. The skin biopsies themselves are flexible; they contain a lot of different cell types meaning there are many pathways that can be activated. A common approach is to investigate disease pathways in human skin biopsies to understand pathophysiology and/or test article behavior. Although highly translational, the throughput for these systems is good, especially for normal skin which comes via the surgical route,. As with most ex vivo experiments, the list of possible endpoints is almost endless.
How long healthy skin can be cultured ex vivo
How long skin biopsies can be cultured ex vivo is dependent on the media change regime and the size of the biopsies. Generally, human skin can be kept "alive" for approximately one week in culture. However, during that week the cells and the epithelium do change, so we recommend completing experiments within four days, with less than 72 hours being optimal. There are various methodologies for modeling human skin ex vivo; however, we recommend always maintaining samples at the air-liquid interface, where the epidermis is exposed to air and the dermis lies within the underlying media.
Punch biopsies from patients with skin disease
Punch biopsies from patients with skin disease are often used to investigate the anti-inflammatory effects of drugs. For this type of study, we recommend designing a 24 or 48-hour experiment. When the samples arrive from the clinical site, they should be placed in a plate with culture media at the air-liquid interface. Your chosen test articles can then be added and incubated with the samples during the culture period. Once the culture period has finished, the supernatants can be harvested to measure cytokine levels, and the biopsies can be stabilized for gene expression analysis. In figure 2, we have included an example of results from this kind of ex vivo study.
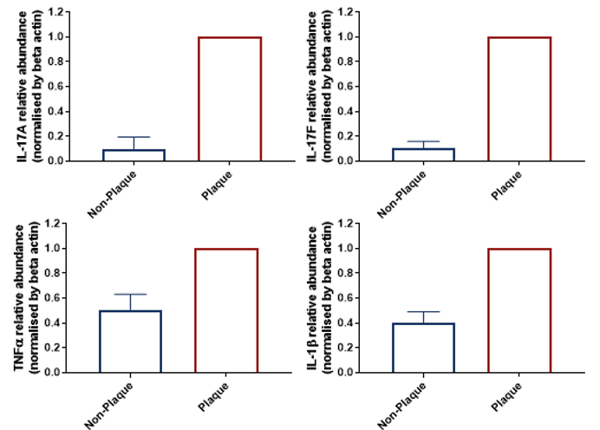
Figure 2: Levels of inflammatory markers vary between non-lesional and lesional psoriasis biopsies. This graph shows mean data across four donors. The gene expression profile is very different between both types of biopsy, would be expected. Although the data shows non-plaque versus plaque skin biopsies, the protocol could be adapted, for example, to investigate drug-treated versus non-drug treated biopsies.
Surgical normal skin tissue
Normal skin samples sourced residual to surgery are a lot larger than dedicated (clinical biopsy) samples, which provides more flexibility in terms of biopsy size and throughput. Punch biopsies made from these resections may not naturally display a disease phenotype; however, they do contain immune cells that can be stimulated to activate pathways of interest. By adding artificial stimulants it's possible to mimic a disease phenotype in healthy skin biopsies.
For example, when creating an AD model, it would be biologically-relevant to target the Th2 pathway with the aim of creating a tissue phenotype that resembles the inflammation seen in AD (figure 3). After induction of inflammation, the effect of novel test compounds in modulating this pathway can be explored. Test compounds are usually applied to the culture media to mimic systemic administration; however, they can also be applied topically on larger biopsies. Following incubation of the compound with the cocktail and test article, the change in inflammatory cytokines levels can be estimated using molecular analysis as specified for diseased biopsies.
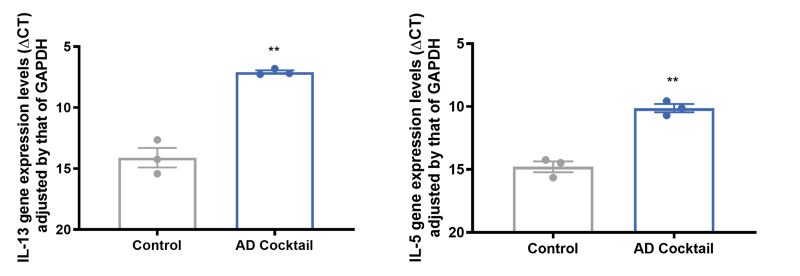 Figure 3: Healthy skin can be induced to produce an AD phenotype using a stimulating cocktail of chemicals. Changes that happen to IL-13 and IL-5 gene expression are hallmark changes you would expect to see in Th2 pathway activation. Not only do we see an increase in cytokines release, but we also see upregulation of IL-13, IL-5, and IL-22 with the cocktail.
Figure 3: Healthy skin can be induced to produce an AD phenotype using a stimulating cocktail of chemicals. Changes that happen to IL-13 and IL-5 gene expression are hallmark changes you would expect to see in Th2 pathway activation. Not only do we see an increase in cytokines release, but we also see upregulation of IL-13, IL-5, and IL-22 with the cocktail.
3D skin cell culture using skin biopsies
A key benefit of human skin biopsies is their complexity, which allows the measurement of multiple endpoints and the investigation of several drug mechanisms and pathways. But for some applications, this complexity can result in background activity that makes it difficult to obtain a good assay window. In this case, you may want to look at a simpler system such as a 3D skin model. Although simpler than ex vivo modeling, 3D skin culture models are higher throughput and possess superior complexity to their 2D counterparts.
Human skin biopsies are an ideal cell source for 3D skin models; not only do they add to the clinical relevance of models, but you can compare the function of diseased cells versus non-diseased cells. A variety of primary cell types can be isolated from human skin, and there are many isolation protocols available. The most common cell types using in 3D skin models include fibroblasts and keratinocytes.
Tips for creating a clinically relevant in vitro skin model
When building a 3D cell culture model, maintaining the external cell environment is critical. There are significant differences in cellular function when in vitro cells are structured correctly in their native extracellular matrix (ECM). We therefore recommend using a 3D cell scaffold for your model, and not adding any additional ECM components other than those made by the cells themselves. Skin fibroblasts will deposit native ECM within the scaffold over time, without needing to add additional ECM components that can change normal fibroblast or epithelial cell function. However, if you want to accelerate ECM formation, adding TGFβ will encourage collagen deposition. Once the dermis is formed, keratinocytes isolated from the same donor can be added to create an overlying epidermis. Other cells, such as melanocytes or cancer cells, can also be added at this stage if the aim is to investigate UV exposure or skin cancer treatments. Figure 4A highlights how TGFβ1 can increase ECM deposition compared to the control, while figure 4B shows how 3D skin models can be used to characterize and quantify compound response.
| A | 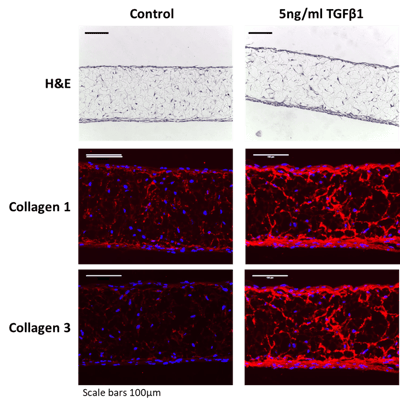 |
B | 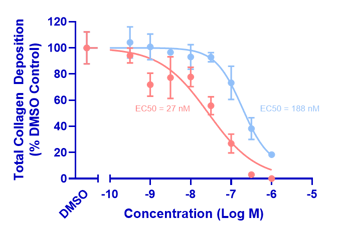 |
Figure 4: TGFβ1 can be added to skin models to increase collagen deposition and test compounds. A, Adding TGFβ1 to fibroblasts cultured in a 3D scaffold can increase collagen deposition; B, Here we've tested two test compounds. They have been added at the same time as the TGFβ1, resulting in a concentration-dependent reduction in collagen deposition over time.
Example of a 3D skin model created using Alvetex
At REPROCELL, we use our the 3D scaffold technology, Alvetex, to build layered stratified epidermal models with a dermis, epidermis, and keratinized top layer. Figure 5 shows an image of this model compared to an ex vivo skin biopsy. It contains two primary cell types: fibroblasts and keratinocytes but other cell types such as immune cells or nerve cells can also be included.
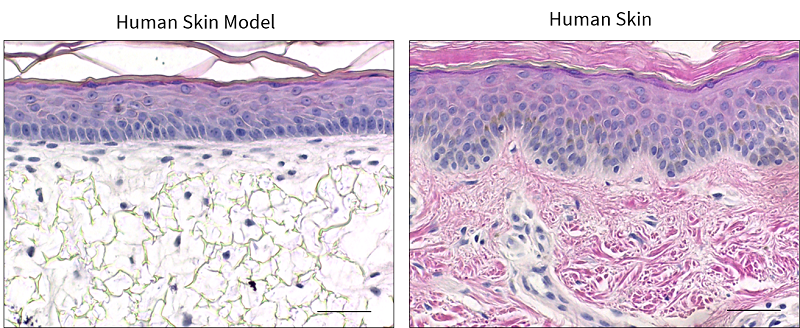
Figure 5: The microscopic structure of a 3D skin cell model made using Alvetex (left) compared with an ex vivo human skin biopsy (right).
Looking to outsource your skin disease research?
We hope that this article has given you an idea of the types of outputs you can get from skin models made using human skin biopsies. If you are looking to outsource your skin research, REPROCELL's skin tissue access has been developed to address as many research areas as possible. So far we have recruited over 280 donors for the completion of over 45 skin studies at our Centre for Predictive Drug Discovery. The network is an extremely useful component of our pre-clinical skin-based research options. You can find out more about our range of ex vivo and 3D bioengineered tissue models here.



.jpg?width=1000&height=562&name=Untitled%20design%20(10).jpg)



