Recently, the microbiome and its role in disease, particularly Inflammatory Bowel Disease has been the focus of much global attention. As our knowledge expands, could this plethora of research be harnessed to help understand the host response to medications? Manipulation of the host's gut microbiome could provide relief from the debilitating symptoms of IBD, whilst sequencing the genome of the organisms colonizing these niche environments may open up new drug development avenues for pharma.
What is the microbiome?
The human microbiome plays a crucial role in health status, and the gut harbours a diverse and host-specific gut microbial community. This niche environment is dominated by five bacterial phyla1: Firmicutes, Bacteriodetes, Proteobacteria, Actinobacteria and Verrucomicrobia. Proportions of these phyla can vary considerably depending on a plethora of factors including the host’s age, immune status and whether they are receiving antibiotic treatment. A direct causal relationship is yet to be established, however the general consensus is that IBD is associated with a dysbiosis in the microbiome. Approaches aiming to restore the microbiome have been investigated and this holds the potential to become the next area of focus for precision medicine.
The influence of the microbiome on inflammatory bowel disease
A genetic component has been postulated to play a role in the development of IBD, with genome wide association studies (GWAS) identifying more than 200 potential susceptibility loci. of additional interest is how the microbiome can also be indicative of disease. IBD encompasses Crohn’s Disease (CD) and Ulcerative Colitis (UC) which are both debilitating immune-related conditions that currently have no cure, with limited therapies or surgical resection being the only treatment option to alleviate symptoms.
Recently a dysbiosis in the gut microbiome has been correlated with these conditions and treatments targeting the microbial balance have been shown to lessen symptoms. Precision editing of the microbiome by developing treatments that target specific organisms has been achieved2. One group of researchers created a chemically induced colitis model which resulted in Enterobacteriaceae expansion and an increase in metabolic pathways essential for its overgrowth. Subsequent targeted inhibition of these pathways resulted in restricted growth and colitis-associated inflammation was reduced in animal models by up to 90%.
Studies suggest that the microbiota is strongly associated with the pathogenesis of IBD. Patients suffering from IBD typically present with a reduced diversity in their microbiome with lower levels of Firmicutes. Reduction in abundance of Faecalibacterium prausnitzii has been reported in patients suffering from CD compared to healthy controls3 and was also found to be correlated with risk of relapse of ileal CD after surgery. F. prausnitzii is known to infer anti-inflammatory effects by increasing IL-10 production4, which inhibits production of inflammatory cytokines IL-2 and IFN-γ.
In addition, an increase in Proteobacteria has been observed in CD patients. Escherichia coli, particularly adhesive-invasive E. coli (AIEC), which exhibits pro-inflammatory properties was found to be the colonise 38% of patients with active CD compared to 6% of healthy subjects5. Causality has yet to be established however these figures show a clear link between the pathogenesis and alteration of the gut microbiome.
A
B
Figure 1. Histopathology of diseased colon with typical Crohn's (A) and Ulcerative colitis (B).
Precision medicine and IBD
Precision medicine is a way of targeting treatments to specific patient cohorts or even individuals. This is achieved by assessing clinical histories, demographics, genetics and determining the relationships between these factors. The microbiome could play an important role in stratifying these patients even further, and by investigating the organisms living in an individual’s gut, treatment regimens may be tailored to suit.
The metabolism of certain drugs can be directly affected by the relative abundance of certain species in the gut and could be used alongside pharmacological data to build a better patient profile to aid in understanding interpatient variation in response to different therapies. These microbiome phenotypes can be integrated with ‘omics’ data which will further enhance precision medicine. Such combined approaches could ultimately aid in the development of new therapies and reduce pre-clinical failure, or help patients receive the best quality of care with existing medications. Either way, its inclusion in medicine can only enhance our knowledge of its role in health and disease.

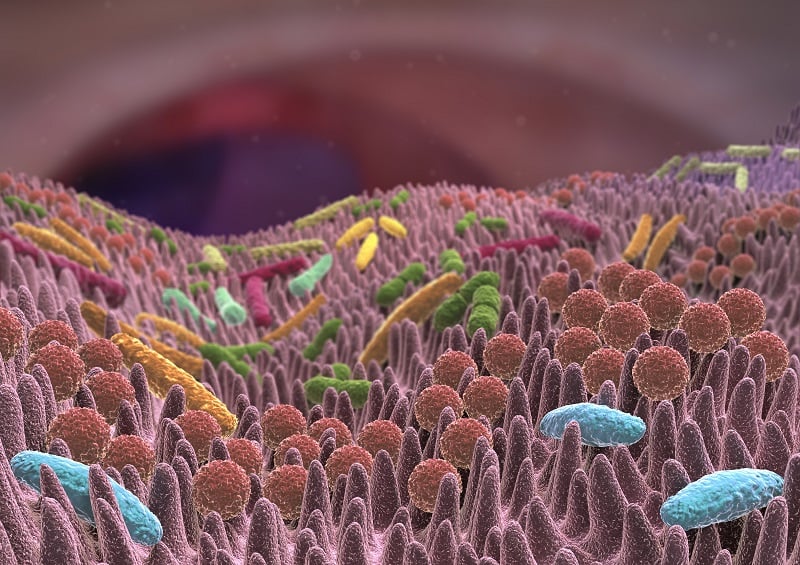
Figure 2. An example of healthy intestinal epithelium
The future of the microbiome and precision medicine
Various strategies have been employed in modifying the microbiome with the aim of restoring it to that of a healthy individual. Faecal microbial transplant (FMT), antibiotics, probiotics as well as direct manipulation of the microbiome therapeutically have all been employed to reduce disease severity. The success of these experiments however, varies.
From a precision medicine perspective, the microbiome could be used as a reliable indicator of treatment efficacy. More research needs to be done however, as it remains unknown whether the change in the microbiome is the direct result of the medication, or from the reduction in inflammation itself. Determining causality may be a challenge and large patient cohorts and longitudinal sampling in the future could provide new insight into associations.
Increasing interest in probiotics, FMT and bacteriophage therapy means that targeting the microbiome of diseases such as IBD could mean a new era of medicine. Moving away from biologics and antibiotics, many of which have a multitude of side effects, could mean a safer way to manage these debilitating diseases. New insights into the microbiome could pave the way for a new era of precision medicine and enhancing our understanding of the complex co-dependent relationship between host and microbes, could mean new diagnostic approaches and therapeutic targets. Find out more about our precision medicine services here.
References
- Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature 486 (2012)
- Zhu et al. Precision editing of the gut microbiota ameliorates colitis. Nature 553 (2018)
- Takahashi et al. Reduced abundance of butyrate-producing bacteria species in the fecal microbial community in Crohn’s disease. Digestion 93:1 (2016)
- Sokol et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA 105:43 (2008)
- Darfeuille-Michaud et al. High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn’s disease. Gastroenterology 127:2 (2004)




.jpg?width=1000&height=562&name=Untitled%20design%20(10).jpg)



